Local hospital officials say they’re prepared as coronavirus reaches New York

As the novel coronavirus continues to spread in the United States — there have been about 100 cases of COVID-19 nationwide, two in New York and seven confirmed deaths—local hospitals are reviewing emergency preparedness plans.
Dr. Sharon Nachman, division chief of pediatric infectious diseases at Stony Brook Children’s Hospital, said Stony Brook Eastern Long Island Hospital in Greenport has and is retroactively reviewing its emergency preparedness plan for respiratory infections in light of the COVID-19 virus.
Dr. Nachman said the emergency preparedness plan was developed in 2009, when the novel influenza A strain (H1N1) emerged.
“It’s been revisited multiple times over the years, when Ebola was an issue,” she said. “Everyone knows where to go, where triage happens, who’s sick enough to go to the emergency room versus triage in their homes, where masks are distributed, how to get them, washing hands. The plan is very comprehensive and we are not unique. Every institution has such a plan.”
Dr. Nachman stressed that while caution and prevetive measures are critical with this virus, it is important to recognize that more people died from the flu last year alone than have succumbed thus far to COVID-19. Every hospital, she said, understands infection control, which symptoms to look out for, how to isolate patients and how to medically care for sick patients.
“Viruses don’t recognize country borders,” she said, “and as good as we can do with restricting travel, because we don’t have a marker for asymptomatic infection, we know who’s sick, but we don’t know who’s well. Are they still infected and perhaps still contagious?”
This, she said, is a question that is difficult to answer as many COVID-19 positive patients are presenting as asymptomatic. While Long Island has not yet seen any cases of the virus, the Centers for Disease Control and Prevention have publicly stated that it is not a matter of if the virus will hit, but when – and it has.
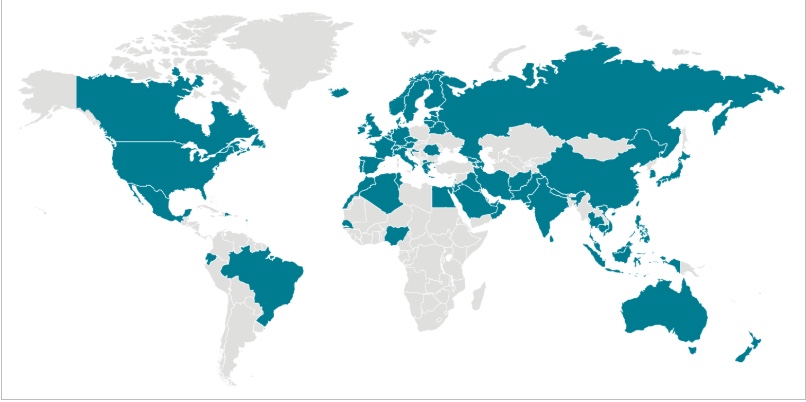
Since the first reported COVID-19 case late last year, what began in Wuhan, China, has spread to South Korea, Iran, Italy, France, Germany and now the U.S. Worldwide figures as of late Tuesday from the World Health Organization show over 90,000 cases in 71 countries and 3,000 deaths. About 95% of the fatalities have been in China. Children, Dr. Nachman said, so far seem to be protected — but that can always change.
Where to find more info
“Looking at the data from China, yes, there were many deaths and many hospitalized, but there was even a volume more that were infected and asymptomatic-well,” Dr. Nachman said. “We expect that type of scenario will play out in every country. Because this is a novel virus, it is likely that you will have protection from it, but having said that, it is also less likely that you will be sick enough to go to the hospital. It is much more likely you will be well, or mildly sick, or you never have a symptom.”
Amy Loeb, R.N., deputy executive director of Peconic Bay Medical Center, agreed that the way the virus is presenting itself is not dissimilar from the flu.
“We are, by nature of being a hospital and dealing with these sorts of illnesses, very well prepared at base line,” she said. “The fact that we’ve had, in New York, the benefit of watching this unfold globally has helped us. From the front door at our hospital and all of our outpatient physician practices and urgent care [centers], we obviously have signage. That’s our first line of informing patients to let us know immediately if they have any symptoms of concern and/or travel.”
In addition to the public awareness piece, PBMC doctors are screening patients according to their symptomology and recent travel history, following protocol in terms of masking potentially exposed patients and isolating them to assess risk. PBMC is continually evaluating its capacity and equipment, monitoring supply levels on a daily basis to ensure adequate volume should the hospital see any infected patients, Ms. Loeb said.
“The health system has activated its emergency management system and there is just constant communication around what’s happening,” she said. “We also are obviously communicating with the New York State Department of Health if we have any patients that we are concerned about. It’s very, very worthwhile to note — both globally and what we expect to see here — that most patients will not require hospitalization. We expect that most patients will be recovering at home, much like with the flu. So, it’s important that we appropriately triage and have patients go home when it’s appropriate.”
The CDC lists symptoms as fever, cough and shortness of breath, all of which may appear anywhere from two to 14 days after exposure. Reported symptoms, it says on the CDC website, have ranged from mild to severe, along, of course, with multiple cases ending in death. The state health department adds to that list runny nose, headache, sore throat and a general feeling of being unwell.
“Immediately, as soon as somebody reports a fever and any sort of upper respiratory or respiratory illness, we would immediately put on a mask and put them in a room,” she said. “That gives us the opportunity to say, ‘Have you been around somebody who has been diagnosed with coronavirus? Have you traveled to any of the places on the current list of interest?’ We ask those questions and if we find that, according to the DOH and CDC, they meet criteria, then we immediately call the Department of Health and they provide guidance on whether or not to test.”
Ms. Loeb said PBMC has not seen an influx of “worried-well” patients, as she describes them — those who are concerned they may be infected, but have no related symptoms and have not traveled or been around anyone infected persons. Isolation and self-quarantining, both health professionals said, is an extremely effective measure.
Dr. Nachman said worthwhile prevention measures include avoiding being around people who are sick, staying home if under the weather rather than going to work and risking infecting others and covering the mouth and nose when coughing or sneezing.
“This is a respiratory illness and we expect it will play out similar to other respiratory infections,” she said. “You will have a runny nose, you may cough, you may have some fever, you may feel under the weather. If you are not sick — and assuming coronavirus is here and it’s an epidemic and we’re seeing it — if those are your symptoms and you are well, I suspect, most people will be encouraged to stay home and take it easy, not go to the emergency rooms and not fill up the emergency rooms because we want to save critical resources for those who we need to decide to admit or not admit. I want to say politely, the hysteria of ‘I may be infected,’ but you’re well should not trigger a visit.”
The hospitals are ready, she said.
“We are well prepared, we are well-equipped, we are well-educated, confident, competent and comfortable managing anything like this, be it influenza or coronavirus,” said Ms. Loeb. “We continue to monitor the situation on a minimum of a daily basis and remain prepared and optimistic about our ability to handle whatever comes at us. That said, it’s our hope that we, as a community, are spared from any major impact, but if it should come, we are prepared.”







