Street medicine team provides health care — and hope
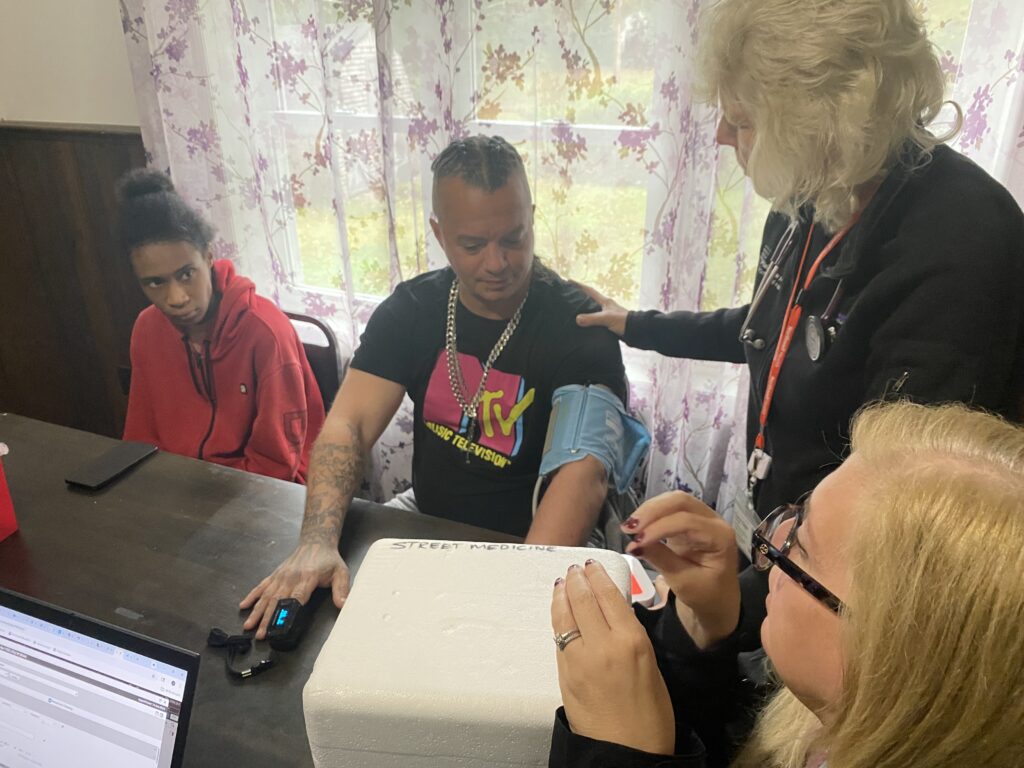
The house is set off the road, hard to find unless you’re looking for it. The people who live here are transitioning from many situations — but today the common area serves as a temporary exam room for the street medicine team at Northwell Health in Riverhead and their partners at Long Island Coalition for the Homeless.
Two clients being housed in Ridge after a year on the streets gather around the kitchen table with hospital staff on one side, clients on the other and the coalition liaison at the end. The questions mirror any routine checkup: John Santomauro, 45, of Selden, worries about weight gain and medications; Natasha Rodriguez, 28, of Baldwin, needs to gain weight.
Both have worked with the street medicine team before, part of a mobile program that brings healthcare directly to unhoused individuals who struggle to access traditional medical care.
“They just gave us everything we needed,” Mr. Santomauro told the Riverhead News Review, which accompanied the medical team. “I’m getting help now for pre-diabetes. I can’t say nothing bad because they’ve just done everything for me.”
Ms. Rodriguez said homelessness interrupted her medical care until the coalition made the connection.
“When we became homeless, we really stopped going to doctors,” she said. “When we bumped into the coalition, they hooked us up with the Northwell team.”

Most street medicine clients are older and covered by Medicaid, so insurance isn’t the problem. Access is. The team arranges transportation, makes referrals, and fills medications for people who lack documentation, transportation or knowledge of how to navigate the medical system.
“We’re really that connection,” said Mary Mahoney, a nurse practitioner with the street medicine team. “It’s not about just us seeing them. It’s about getting them into the system so that they’re not continuing to rely on the emergency department for care.”
Another large part of what the street medicine team does is build trust. Vulnerable populations often neglect medical care, but seeing how much the team cares about their well-being pushes clients to follow through on recommendations.
“We’ve had people who have refused medical care who, after getting expert advice, have actually turned around and said, ‘Yes, I’m willing now to go to the hospital,'” said Greta Guarton, executive director of LICH.
That trust starts with Dylan Schwarz, the LICH liaison who screens clients and builds a rapport before arranging medical visits. In general, people who have spent any time unhoused are experiencing medical issues due to the harsh living conditions.
“Someone who has diabetes, but it’s well controlled, they’re not going to need the same kind of care as someone who has diabetes that’s ravaging their body,” Mr. Schwarz said. “Instead of us trying, and perhaps struggling, to get them back in to their primary to get the specialist, we can just refer them right to that specialist. In certain cases, even with the clients having providers, having a prescription kind of on the spot has been helpful.”
Many housing programs require health screenings to qualify, so it is critical for clients to be seen.
“People are able to get treated and remain much healthier,” Ms. Guarton said. “It moves them much faster toward being able to make a change in their lives.”
Mr. Santomauro and Ms. Rodriguez have made significant progress since connecting with the program, allowing them to focus on rebuilding other areas of their lives.
“I trust them. They’re helping a lot of people,” Mr. Santomauro said. “They should get recognition, because I’m very happy.”









